Boy died after signs of deadly infection were missed at ‘very busy’ hospital
Hospital says it is taking coroner's findings seriously
Thursday, 15th August 2024 — By Tom Foot

Daniel Klosi with his mother Lindita Alushi
VITAL signs of a deadly infection in an autistic boy were missed at the Royal Free – despite his parents bringing him in to A&E for help four times, an inquest heard.
Coroner Mary Hassell ruled Daniel Klosi would not have died from Strep A sepsis, just after midnight on April 2 last year, had procedures been properly followed in a “narrative” determination at Poplar Coroner’s Court yesterday (Wednesday).
The four year old’s parents, from Kentish Town, were left in tears at the end of a gruelling two day hearing that exposed a series of failings and has led to a rethink in the way child patients with autism are assessed.
Dr Gautham Benoy had only been working in the Pond Street hospital’s paediatric department for two months when he was called down to the emergency department to help an over-stretched team on an unusually busy Saturday in A&E.
The trainee doctor did not realise that Daniel – who had finally been admitted after being sent home by hospital staff three times, including earlier that morning – was already septic.
Dr Benoy told the court: “I could see he was an unwell child. My experience was limited, but I had seen septic children. He did not appear like the children I had seen. He did not seem lethargic. He was alert. There was no rash. I thought his symptoms were localised, not systemic. I did think he was at risk of sepsis.”
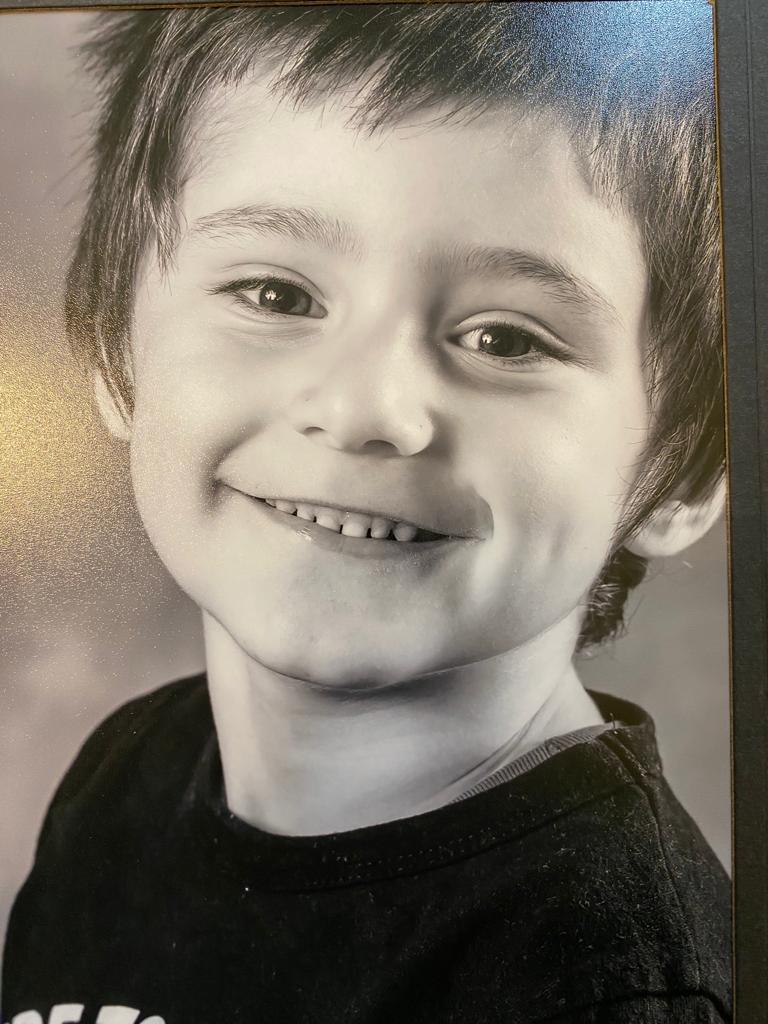
Daniel Klosi
“I’m sorry for everything you have been through,” Dr Benoy told Daniel’s parents in his evidence.
The inquest heard how it took four hours from the time Daniel was admitted for the severity of his condition to be realised by consultants due to a series of problems, including incomplete triage notes, delays in taking blood tests, heart rate and temperature checks, X-rays – and the failure to connect a cannular Daniel needed to administer crucial antibiotic treatment.
Dr Benoy told the court that a trolley with equipment for making basic patient “observations” on Daniel – including taking temperatures and bloods – was not available to him in the A&E.
The inquest repeatedly heard about a disconnect between his parents view on how sick he was and the hospital’s clinicians.
One reason for the lack of lethargy – one of the main symptoms of sepsis – shown by Daniel when assessed by doctors could have been that the bright lights and scary noises the department were “activating” his autism.
With the deadly infection flying under the radar, A&E consultants attended to patients they believed were more ill than Daniel.
SEE ALSO LITTLE DANIEL’S PARENTS WERE SENT AWAY FROM A&E – JUST HOURS LATER HE DIED FROM SEPSIS
Dr Amisha Singh told the court: “It was very busy. What was unusual was how unwell so many of the patients were. I thought I was seeing the sicker patients, going on the information I had. A clinical reason [to see Daniel] hadn’t been flagged to me.”
She told the court that she had considered calling for a third consultant to come in to work from home, given the pressure that evening, but had decided against it.
Asked by coroner Mary Hassell if Daniel was already septic at the point of his fourth admission – four hours before the condition was diagnosed – she said “yes, he would have been septic”.
Sepsis – where the body attacks itself in response to an infection – is sometimes referred to as the “silent killer” and is notoriously difficult to diagnose. It is relatively simple to treat if caught in time, with antibiotics, the court heard.
The inquest heard that the point when antibiotics would likely have saved Daniel’s life was on the third attendance – the morning of April 1. But this time the parents were sent home and told to try Calpol, and a consultant “failed to read medical records” that showed he had been brought in two times already.
In her narrative determination, Mary Hassell said: “They failed to appreicate the illness had been going on for a week. If they had, it would have led to blood tests, and this would have led to antibiotics. Daniel’s life would have been saved.”
SEE ALSO COUPLE ARE HEARTBROKEN TO SEE SEPSIS TRAGEDY REPEAT AGAIN AND AGAIN
She said that Daniel’s death had in part been caused by an “atypical” version of sepsis, which had not shown itself in a normal way.
Dr Tim Wickham, a paediatrician at the hospital who carried out an investigation into the case, said changes were being introduced at the hospital following the “failings”. Patients with “incomplete observations” like Daniel will be “flagged” up to senior consultants.
Reattending patients would be bumped up to the top of the queue of those waiting for treatment, he added.
Dr Wickham said the case had made the hospital team think about how they approached austistic patients as “maybe the real Daniel was not the one we were seeing”.
In a strange twist to the story, a crucial passage of CCTV footage that the family had requested from the hospital as part of their case was mysteriously deleted after a long-running dispute about whether it would be made available.
Daniel’s father Kastriot Klosi said in a statement: “I never felt listened to. The doctors were fixated on it being another virus. They said his skin and breathing looked fine. He was struggling, we were asking for help.”
Mother Lindita Alushi – a pharmacy worker and qualified doctor in Albania – said: “Every day we wonder if more could have been done to save our little boy.”
Speaking to the New Journal last year in the week of the tragedy she told how her son “loved cooking, animals and playing with his marbles”, and was enjoying life in the Ferdinand Street nursery.
A Royal Free spokesperson said: “This is a desperately sad case and we are deeply sorry that Daniel died while under our care.
“We would like to share our heartfelt condolences with his family and loved ones.
“We identified a number of areas for improvement, and measures were taken to immediately address these.
“This included improving training and awareness for all of our staff, particularly in relation to children who repeatedly visit our emergency departments; how we care for children with learning disabilities; and the importance of listening to parents and carers when they raise concerns.
“We take the coroner’s findings seriously.”